Coeliac disease a condition in which there is an intolerance of the protein gluten, found in grains such as wheat, rye and barley. The intolerance causes a flattening out of the finger-like projections in the small intestine, which dramatically reduces the surface area of the gut available for absorbing nutrients from our diet. Not surprisingly, therefore, those with coeliac disease who go undiagnosed for an extended period of time can end up malnourished and underweight.
One could argue that coeliac disease starts in the gut, and there’s no doubt that it can cause gastrointestinal symptoms including bloating, wind and digestive discomfort. But the condition can give rise to many other symptoms too, many of which are unlikely to be put down to as ubiquitous a food component as gluten. Here’s a list of potential symptoms from the coeliac.org. uk site:
- diarrhoea, excessive wind, and/or constipation
- persistent or unexplained gastrointestinal symptoms, such as nausea and vomiting
- recurrent stomach pain, cramping or bloating
- any combination of iron, vitamin B12 or folic acid deficiency
- tiredness and/or headaches
- weight loss (but not in all cases)
- mouth ulcers
- hair loss (alopecia)
- skin rash (dermatitis herpetiformis (DH))
- tooth enamel problems
- osteoporosis
- depression
- infertility
- repeated miscarriages
- joint and/or bone pain
- neurological (nerve) problems such as ataxia (poor muscle co-ordination) and neuropathy (numbness and tingling in the hands and feet).
A few weeks ago I was speaking at an event and spent some time talking with a woman who has vast experience in coeliac disease. She told me that most common symptoms of coeliac disease are actually neurological in nature – a category which comes up last in the list on the coeliac.org.uk site but perhaps should be first.
I was interested to see a study just published in the American Journal of Gastroenterology which estimates that 1.8 million Americans suffer from the condition, as diagnosed by bloods tests (positive immunoglobulin A tissue transglutaminase and immunoglobulin A endomysial antibodies) [1].
Here’s a statistic that concerned me though: 1.4 million (78 per cent) of them don’t know they have the condition. Given the fact that coeliac disease presents in so many (and perhaps so many unexpected ways), it’s perhaps not much of a surprise that the condition can so often go undetected.
However, there’s another side to this issue that I think needs recognising. Just because someone comes up negative on blood tests for coeliac disease, does not necessarily mean they don’t have a problem with gluten. This is not just my opinion or clinical experience, by the way, as Australian research published last year shows it [2].
Another interesting thing about this recent study is that it assessed whether or not individuals were eating a gluten-free diet (or not). It was found that about one in every 160 people had adopted a gluten-free diet, though in about 80 per cent of these, there was no formal diagnosis of coeliac disease.
This finding is perhaps not surprising, seeing as it is possible for individuals to have symptoms of gluten intolerance in the absence of coeliac disease. Now, of course, taking gluten out of the diet and feeling so much better might be down to the placebo response and not due to relief from a genuine problem with gluten. However, even if this were to be the case, I personally have no issue with it. For me (and practically every patient I have ever met) it’s relief that is being sought, and it’s generally welcome whatever the precise mechanism through which it may have come.
Now, sometimes you’ll hear health professionals warning of the hazards of self-diagnosis. The notion here is often that ‘cutting out a whole food group’ is hazardous, and will leave people deficient in key nutrients. Like what, I would ask? What do grains like wheat and rye provide for us that cannot be obtained adequately and more healthily elsewhere? And it should go without mention, here, that grains such as wheat are rich in substances called phytates that impair nutrient absorption. Even if grains were über-nutritious (they are not), they do not necessarily give these nutrients up easily to the body.
I’ve found through experience that when someone takes out gluten-containing grains (or grains generally) from their diet, there is a good chance that they will experience a host of benefits in terms of health and general wellbeing.
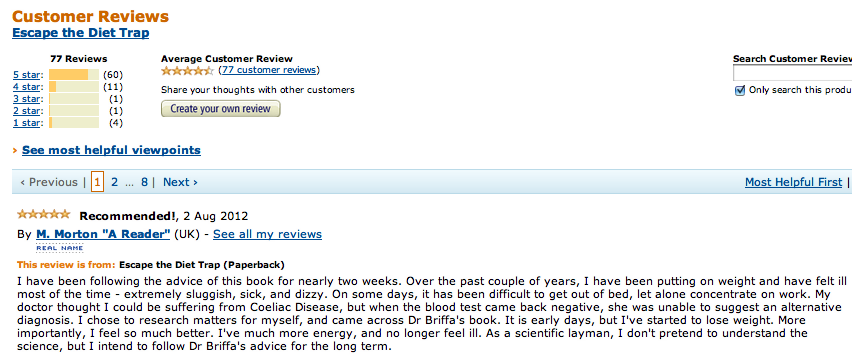
Below is a screenshot of an amazon review for my book Escape the Diet Trap that came in today followed by the text from the review. In short, the reviewer had several non-specific symptoms which his GP (family doctor) suspected might be down to coeliac disease, but the test came back negative. He ended up doing his own research changing his diet and, if he took the advice in my book, would have excluded grains including those containing gluten. In a couple of weeks, he already feels much better and no longer feels ill.
It is impossible to say what, specifically, about his change in diet has led to him feeling better, or if it’s a placebo response or something else. However, if it turns out that this man has a sensitivity to gluten which was not picked up by standard blood tests, then I would not be at all surprised.
I have been following the advice of this book for nearly two weeks. Over the past couple of years, I have been putting on weight and have felt ill most of the time – extremely sluggish, sick, and dizzy. On some days, it has been difficult to get out of bed, let alone concentrate on work. My doctor thought I could be suffering from Coeliac Disease, but when the blood test came back negative, she was unable to suggest an alternative diagnosis. I chose to research matters for myself, and came across Dr Briffa’s book. It is early days, but I’ve started to lose weight. More importantly, I feel so much better. I’ve much more energy, and no longer feel ill. As a scientific layman, I don’t pretend to understand the science, but I intend to follow Dr Briffa’s advice for the long term.
References:
1. Rubio-Tapia A, et al. The Prevalence of Celiac Disease in the United States. The American Journal of Gastroenterology. 2012 Jul 31. doi: 10.1038/ajg.2012.219. [Epub ahead of print]
2. Biesiekierski JR, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106(3):508-14